INTRODUCTION
The patient with post-zoster neuralgia after herpes zoster infection suffers from constant pain and episodic pain, and the individual is disabling to daily living. However, it is often inadequately managed for chronic pain yet [2]. Because Neuropathic pain is additionally heterogeneous and definite with constant and episodic pain, treatment of episodic pain with constant pain must have an adequate therapeutic approach to relieve pain following the patient's circumstances. Recently guidelines recommend that the first medical treatment of postzoster neuralgia is represented by using gabapentinoids as needed [4]. Several studies show that the combination treatment of injection to scar and ICNB for patients with post-zoster neuralgia is effective [13]. We demonstrate whether the combination treatment of injection to scar and ICNB is safe and effective in management for patients with post-zoster neuralgia on the thorax by evaluating the change in VAS and daily morphine consumption.
MATERIALS AND METHODS
1. Subjects
We collect retrospective data on 23 patients undergoing combination treatment of injection to scar and ICNB in the management of neuropathic pain in patients with post-zoster neuralgia on the trunk during eight years beginning on January 1, 2011. Among 23 patients, 10 were male, and 13 were female, ranging between 13 and 79 years old (61.65±17.35: Mean±SD). Sixteen patients had a location of pain on the right and seven on the left. The lesion was mostly single, and multiple lesions were observed in five patients. In consequence, among patients with post-zoster neuralgia, the patients were caused by herpes zoster infection and after the antiviral agent treatment. These patients additionally complained of heterogeneous and robust pain in chest and upper back on the thorax with features such as vague, burning, and sharp nature and did not respond to medication with gabapentinoids in constant and episodic pain. Also, they did not show response to medication with rapid-onset or short-acting opioids for episodic pain. Patients were treated with medication for 3 months up to 126 months (12 months: Median). The characteristic of patient groups treated by the combination treatment of injection to scar and intercostal nerve block is summarized in Table 1. Pain intensity measured using VAS, Quality of life scale (American Chronic Pain Association), and gabapentin and morphine consumption were measured at baseline and after the combination treatment of injection to scar and ICNB. The patient was scheduled to return to the outpatient clinic after one week during the six months follow up visits after the combination treatment of injection to scar and ICNB.
2. Therapeutic Method
1) Inclusion Criteria
The primary indication for the combination treatment of injection to scar and ICNB is to alleviate pain from dermatome by the ICN. Treatment of post-zoster neuralgia is complex, often requiring multiple approaches. Clinical trials have shown that opioids, tricyclic antidepressants, and gabapentin reduce the severity or duration of post-zoster neuralgia, either as single agents or in combination. The adverse effects of these medications can be addictive, especially in elderly patients. The topical application of lidocaine patches or capsaicin cream can provide relief for some patients. We started the combination treatment of injection to scar and ICNB for patients with postzoster neuralgia on the thorax when the described treatment fails to control more than 50% of the pain or when side effects from medication occur.
2) Procedure
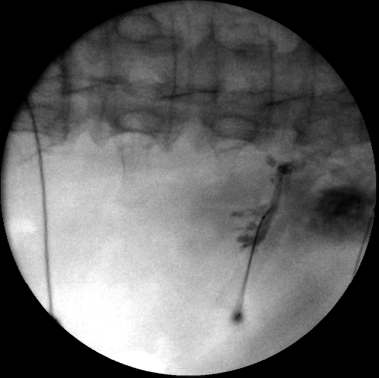
The patient is prepared at the operating room in a sterile manner, and the patient was placed lying prone position to maintain lordosis, and the position was maintained with a pillow beneath the abdomen. The surgeon confirmed and marked reference points: Spinous process of thoracic vertebrae, ribs, the dorsal midline, including the lateral edge of the vertebral body before the ICBN. The ICN can be blocked anywhere proximal to the midaxillary line, where the lateral cutaneous branch takes off. The block is commonly carried out at the posterior axillary line or just lateral to the paraspinal muscles, at the angle of the rib. In adults, the most common site for ICNB is at the angle of the rib (6-8 cm from the spinous processes. At the angle of the rib, the rib is relatively superficial and easy to palpate, and the subcostal groove is the widest. The nerve is inferior to the posterior intercostal artery, which is inferior to the intercostal vein. Blocking intercostal nerves medial to the angle of the rib is not recommended because the nerves lie deep to the posterior intercostal membrane with very little tissue between it and the parietal pleura and the overlying thoracospinalis muscle makes rib palpation difficult. Once the needles are in a good position, the stylets are removed from the needle, and a small volume of contrast media is injected through the needle hubs. Its diffusion is observed on the fluoroscopic anteroposterior view, and contrast media is confined to the midline and concentrated. The mixture of 3 mL of 0.5% bupivacaine containing 1 mg of triamcinolone and Hyaluronic acid was injected around ICN under fluoroscopy (Fig. 1).
3. Statistical Analysis
fluoroscopic anteroposterior view, and contrast media is confined to the midline and concentrated. The mixture of 3 mL of 0.5% bupivacaine containing 1 mg of triamcinolone and Hyaluronic acid was injected around ICN under fluoroscopy (Fig. 1).Pain intensity measured using VAS, and morphine consumption at baseline and each visit after the combination treatment of injection to scar and ICNB. The repeated measure one-way analysis of variance (ANOVA) is used to determine whether there are any statistically significant differences between the means of baseline and the means of a periodic visit.
RESULTS
1. Pain relief after the combination treatment of injection to scar and ICNB versus Baseline
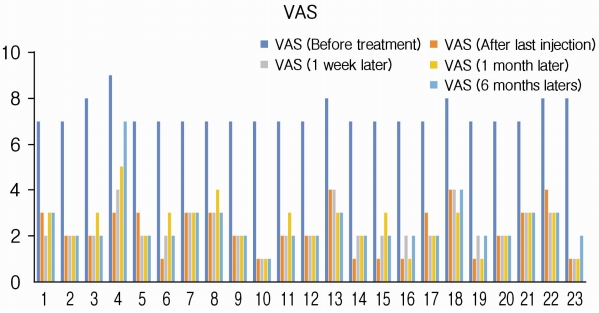
VAS for pain intensity was measured at baseline and visits after the combination treatment of injection to scar and ICNB for patients with post-zoster neuralgia on the trunk. The mean (±SD) VAS of baseline status was 7.3 (±0.56) before the combination treatment in the management of episodic pain with constant pain in patients with post-zoster neuralgia. VAS decreased to 2.26±1.05 after the combination treatment compared with baseline VAS and was sustained by 2.35±0.83 for 1 week and by 2.48±0.99 at 1 month. After 6 months, the pain remained at 2.52±1.16 (Fig. 2) The repeated measure ANOVA was used to determine whether there was any statistically significant difference between the means of baseline and regular visits. Mean difference (2.26±1.05) after treatment: 2.35±0.83 after 1 week: 2.48±0.99 after 1 month: 2.52±1.16 after 6 months) between the baseline VAS (7.3±0.56) and VAS observed during 6 months is statistically significant (p<0.001) during follow-up visit for 6 months (Table 2).
2. Gabapentin and Morphine consumption after the combination treatment of injection to scar and ICNB versus Baseline
Relief of pain after the combination treatment lasts for 1 week, which in most cases, for over 1 month. The combination treatment made it possible to reduce short-acting and rapid onset opioids in morphine consumption, and the baseline doses were 104±126 mg/day that significantly reduced to 40±20 mg/day after 1-month post-procedure (p<0.001). The reduction by 32±17 mg/day in daily morphine consumption was observed at 6 months after the combination treatment compared with the baseline (Table 3). The patient was taking gabapentin (1,200 ±300 mg/day) before treatment. The dose of gabapentin in the first month did not significantly decrease in taking gabapentin (1,000±300 mg/day). Consumption decreased significantly. The mean dose value (±SD) after 6 months was also significantly reduced by 600±300 mg/day.
3. Quality of life scale after the combination treatment of injection to scar and ICNB versus Baseline
QOLS measured at baseline was 4.5±1.6. QOLS (6.7±1.5) after the first 1 week did improve according to pain relief. QOLS by 6.8±1.6 was sustained at 1 month after the treatment compared with the baseline, and QOLS (6.2±1.7) after 6 months was similar to follow-up visits. There was a difference in QOLS after the combination treatment of injection to scar and ICNB versus Baseline.
DISCUSSION
Infection by herpes zoster begins with localized abnormal skin sensations, ranging from itching or tingling to severe pain, which precedes the skin lesions by one to five days [3]. The pain of variable severity occurs in virtually all patients with acute herpes zoster. An erythematous maculopapular rash progresses to clusters of clear vesicles, which continue to form for three to five days and evolve through stages of pustulation, ulceration, and crusting. Healing occurs over two to four weeks and often results in scarring and permanent changes in pigmentation. The cutaneous eruption is unilateral and does not cross the midline [4].
Post-zoster neuralgia (defined as pain that persists more than 30 days after the onset of rash or after cutaneous healing) is the most feared complication in immunocompetent patients. Both the incidence and the duration of post-zoster neuralgia are directly correlated with the patient's age [10,14]. The reported incidence of postherpetic neuralgia ranges from 8 to 70 percent and increases with advancing age [1].
Treatment of postherpetic neuralgia is complex, often requiring a multifaceted approach. Clinical trials have shown that opioids, tricyclic antidepressants, and gabapentin reduce the severity or duration of postherpetic neuralgia, either as single agents or in combination. The adverse effects of these medications can be addictive, especially in elderly patients [10]. The topical application of lidocaine patches or capsaicin cream can provide relief for some patients. In a study of patients with intractable postherpetic neuralgia, intrathecal injection of methylprednisolone acetate once weekly for four weeks resulted in a significant reduction in pain. Additional data are required to validate these promising initial results [4].
In 1971, Epstein demonstrated that intradermal injection of triamcinolone and procaine is an effective treatment for postzoster neuralgia [7]. Since then, there have been a few similar reports. Nerve block, in combination with corticosteroids, is now widely used in the treatment of post-zoster neuralgia [5,6,8]. The first use of intralesional corticosteroid injections would seem to be a reasonable therapeutic measure in herpes zoster since probably neural and perineural inflammation are essential in the development of symptoms.
Sehgal and Gardner treated 12 patients with post-zoster neuralgia by the local injection of hydrocortisone and procaine. They reported results “good” in two and “fair” in five, and “poor” in three patients who were treated by local injection of procaine alone. The reason for subcutaneous injection is to minimize the hazard of cutaneous atrophy, which might add to the scarring caused by zoster in some patients [15]. The accumulation of sodium channels at the injury sites and accompanying inflammation of the peripheral nerve are supposedly responsible for the acute pain of herpes zoster. Lidocaine is thought to act by selective, but only partial, inhibition of voltagegated sodium channels of damaged or dysfunctional un- myelinated C fibers and small myelinated A-fibers [11,15]. Corticosteroids exert an intense anti-inflammatory action, which might minimize nerve damage and thereby relieve post-zoster neuralgia and prevent post-zoster neuralgia [9].
In comparison, the subcutaneous injection of lidocaine and triamcinolone is a safe and straightforward method to block affected peripheral nerves and reduce inflammation. In the literature, the pain NRS scores decreased significantly in all patients with post-zoster neuralgia one month after rash onset. Still, patients who received standard treatment plus subcutaneous injection showed substantially more significant improvement in pain scores than those who received standard therapy alone [5,6].
As hyaluronic acid is highly hydrophilic, it is a polymer that is well suited to applications requiring minimal cellular adhesion. Postoperative adhesions, which form between adjacent tissue layers following surgery, impede wound healing and often need additional surgical procedures to be repaired successfully. Barriers made from cross-linked hyaluronic acid have been effectively used to prevent such adhesions from forming and is naturally present in high concentrations in the skin and soft connective tissues. Therefore, hyaluronic acid is an appropriate choice for a matrix to support dermal regeneration and augmentation. Hyaff scaffolds cultured in vitro with keratinocytes and fibroblasts have been used to create materials similar to skin, including two distinct epidermal and dermal-like tissue layers. Moreover, as a result of its ability to form hydrated, expanded matrices [12].
CONCLUSION
In conclusion, this clinical study suggests that the combination treatment of injection to scar and intercostal nerve block for patients with post-zoster neuralgia on the trunk of the mixture of 3 mL of 0.5% bupivacaine containing 1 mg of triamcinolone and hyaluronic acid in combination with standard treatment (gabapentinoids, TCA and analgesics) is effective and safe for treating episodic pain with constant pain caused by herpes zoster infection and for relieving post-zoster neuralgia. A largescale multicenter clinical trial is needed to confirm our findings.