Risk Factors for Recurrence of Disc Herniation After Single-Level Lumbar Discectomy
Article information
Abstract
Objective
Herniated nucleus pulposus is a common disease of the lumbar spine. Recurrence of disc herniation and subsequent disc degeneration are the most common problems following discectomy. Many first-time lumbar discectomy patients experience favorable outcomes; however, same-level recurrent discectomy can occasionally induce unfavorable results. Therefore, in this study, we retrospectively analyzed the risk factors for recurrence of lumbar disc herniation after discectomy.
Methods
From January 2013 to December 2015, 226 patients underwent one-level discectomy in our department. We excluded patients with less than two years of follow-up, a previous spine deformity with a compression fracture, foraminal or extraforaminal discs, or a history of previous lumbar operation history, leaving 71 selected patients. Patients were divided into recurrent and non-recurrent groups and various factors were retrospectively compared between the groups.
Results
Patients with preoperative disc space narrowing experienced recurrence less commonly; however, this was not statistically significant (10.0% and 25.5%, respectively; p=0.150). A disc height decrease of more than 20% during the follow-up period was a statistically significant risk factor for recurrence (36.4% and 14.3%, respectively; p=0.035), and grades 3 and 4, compared to grades 1 and 2, facet joint degeneration were also statistically significant risk factors for recurrence of disc herniation (41.2% and 14.8%, respectively; p=0.020).
Conclusion
Patients who underwent more than a moderate degree of preoperative facet joint degeneration on the operated side and for whom the progression of disc space height decreased during the follow-up period may require closer observation for recurrence of disc herniation.
INTRODUCTION
Herniated nucleus pulposus is a common disease of the lumbar spine, and discectomy is the standard treatment method for this disease. Recurrence of disc herniation and subsequent disc degeneration are the most common problems after discectomy. While the recurrence rate of disc herniation varies between studies, it is known to be about 5% to 15% [1-4], irrespective of the surgical method. A retrospective study showed that nearly 25% of discectomy patients experience recurrent herniation on follow-up radiographic evaluation; however, most of them are asymptomatic [5]. In 15% to 25% of discectomy patients, back pain recurs after two-year follow-up [6]. Recurrence of disc herniation after lumbar discectomy may re-aggravate back pain, radiating pain, and reduce the quality of life. Recurrence of disc herniation is the primary cause of the poor outcome of discectomy. A more aggressive removal of disc material can not only reduce the recurrence of disc herniation, but can also cause persistent back pain due to endplate damage and acceleration of disc height decrease [3,7]. The differential diagnosis between recurrence of disc herniation and scar tissue formation at the operative site is also essential. Many first-time lumbar discectomy patients experience favorable outcomes; however, same-level recurrent discectomy occasionally induces unfavorable results. Therefore, we retrospectively analyzed the risk factors for the recurrence of lumbar disc herniation after discectomy.
MATERIALS AND METHODS
1. Patient Selection
This study was approved by the Institutional Review Board of our hospital (BOHUN 2020-08-027). From January 2013 to December 2015, 226 patients underwent one-level discectomy in our department. We excluded patients with a follow-up period of less than two years, previous spine deformity with a compression fracture, foraminal or extraforaminal disc, reoperation within six months due to remaining disc, and previous lumbar operation history including the same and other levels. In total, we selected 71 patients. Recurrence of disc herniation is defined as recurrence on the same-level, or on the ipsilateral or contralateral side, at least six months after the primary operation. When the symptoms were affected by daily activity, we assessed the patient’s condition and the level of symptom recurrence. All patients underwent magnetic resonance (MR) imaging before primary discectomy.
2. Analytic Parameters
We analyzed patients’ demographic parameters such as age/sex, smoking history, diabetes mellitus (DM), and body mass index (BMI). Radiological parameters included operated disc herniation level, discectomy side (right, left, or both), change of lumbar disc height during the follow-up period, degree of Modic change, disc degeneration, facet joint degeneration, type of disc herniation, and paraspinal muscle atrophy.
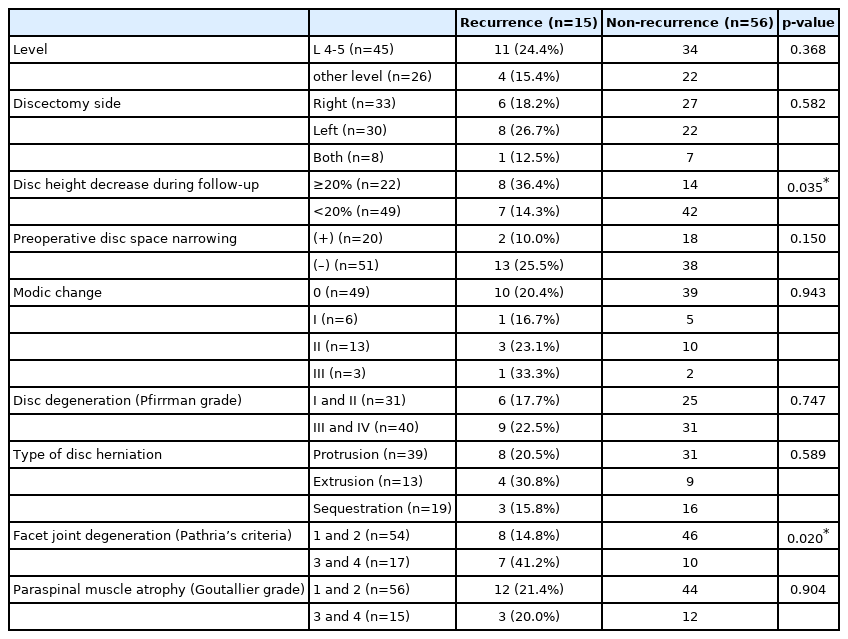
The level of disc herniation was divided into the L 4-5 level and other levels. The side of the discectomy was defined as right, left, or both. Lumbar disc height was calculated by adding the anterior, middle, and posterior disc heights and subsequently dividing by three. We divided the patients into two groups based on whether or not the disc height decreased by more than 20%. Disc space narrowing is defined as reducing disc space height compared to adjacent disc space on the lateral view. Using sagittal T1, T2-weighted image (WI) on MR imaging, the Modic change was investigated by type 0, I, II, and III on the operated level, with type 0 indicating the absence of Modic change. The degree of disc degeneration was classified according to the Pfirrmann classification. It was divided into grades I, II, III, IV, and V. Facet joint degeneration was graded according to Pathria’s criteria and divided into grades 1, 2, 3, and 4 (Table 1). The type of disc herniation was defined as either protrusion, extrusion, and sequestration. Paraspinal muscle atrophy was classified based on the Goutallier grading system on axial T2-WI on the herniated disc level, and was divided into grades 0, 1, 2, 3, and 4.
3. Statistical Analysis
Fisher’s exact test and t-test were used for statistical analysis using SPSS (version 18.0, SPSS Inc. Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
RESULTS
The study included 58 men and 13 women. The mean age was 61.89±13.38 years (range 21–82 years), and the mean follow-up period was 36.90±12.20 months (range 24–70 months). Among the patients, 15 experienced recurrence (21.1%). The mean time for recurrence of disc herniation was 17.47±11.24 months (range 8–46 months). All patients with recurrence underwent reoperation.
1. Demographic Parameters
Of the 71 patients 13/58 male and 2/13 female patients experienced recurrence (22.4% and 15.5%, respectively; p=0.575). In patients aged >65 years, ten patients had recurrence among the 46, and of those aged <65 years, five among the 25 (21.7% and 20.0%, respectively; p=0.864). Smokers experienced recurrence more commonly than nonsmokers; however, the difference was not statistically significant (29.2% and 17.0%, respectively; p=0.236). Patients treated for DM experienced recurrence more commonly; however, the difference was not statistically significant (25.0% and 19.6%, respectively; p=0.617). Non-overweight patients (<25 on the BMI scale) experienced recurrence less commonly than overweight patients (12.0% and 26.1%, respectively; p=0.165) (Table 2).
2. Radiological Parameters
Of the patients who underwent an operation on L 4-5, 11/45 experienced recurrence, while 4 patients experienced recurrence at other levels (24.4% and 15.4%, respectively; p=0.368). The discectomy side was also not related to recurrence rate (right, left, and both: 18.2%, 26.7%, and 12.5%, respectively; p=0.582). A decrease in disc height by more than 20% during the follow-up period was considered a risk factor for recurrence (36.4% and 14.3%, respectively; p=0.035); the mean preoperative disc height was decreased from 11.71±1.69 mm to 9.67±1.86 mm in the recurrence group and 11.16±2.44 mm to 9.89±2.24 mm in the non-recurrence group.
Patients who experienced preoperative disc space narrowing observed recurrence less commonly than those who did not; however, this was not statistically significant (10.0% and 25.5%, respectively; p=0.150). The recurrence rate in the absence of preoperative Modic change patients was similar to that in the presence of preoperative Modic change patients (20.4% and 22.3%, respectively; p=1.000).
Patients with preoperative disc degeneration grades III and IV experienced recurrence more commonly than those who grade I and II (22.5% and 17.7%, respectively; p=0.747). Extrusion-type disc herniation recurred more commonly than protrusion and sequestration type (30.8%, 20.5%, and 15.8%, respectively; p=0.589).
Grades 3 and 4 facet joint degeneration were a risk factor for disc herniation compared to grades 1 and 2 (41.2% and 14.8%, respectively; p=0.020). The degree of paraspinal muscle atrophy was not observed to be a risk factor (grade 1 and 2: grade 3 and 4, 21.4% and 20.0%, respectively; p=0.904) (Table 3).
DISCUSSION
Studies have revealed that various factors can predispose individuals to disc herniation. Disc reherniation is a common cause of symptom recurrence after discectomy. In most cases, when disc reherniation occurs, the symptoms observed before primary discectomy reappear. Differential diagnosis between disc reherniation and postoperative epidural scar formation is also essential, and enhanced MR imaging is helpful for this pulpose [8].
Old age may be a risk factor for increased recurrence of disc herniation [9]. However, other reports have demonstrated that the younger generation with a high disability is at a high risk of recurrence, and a history of previous trauma before recurrence is common [10,11]. One study showed that female patients are more likely to experience recurrence [12]; however, another study contradicted this assertion [11]. Smoking influences cell proliferation, extracellular matrix production, and viability of nucleus pulposus by nicotine effect [13]. It induces disc degeneration and protects annular healing after discectomy, and may also be an important factor in disc reherniation [14].
High BMI, postoperative Oswestry disability index and a high degree of disc degeneration are also risk factors for recurrence of disc herniation [2,9,15,16]. Obesity and type 2 diabetes are important factors for disc degeneration [17]. Thus, favorable outcomes after discectomy are not common in diabetic patients [17]. Obesity is influenced by mechanical overloading of the spinal segment, and hyperglycemia directly affects disc cell viability. Intervertebral disc nutrition may be controlled in diabetic patients due to difficulties in diffusing of nutrients and oxygen delivery through the cartilaginous end-plate [18]. In our study, age, sex, smoking and DM history, and BMI were not independent factors for disc herniation recurrence.
The highest rate of reherniation occurred when large and massive annular defects were observed. Cases of extruded disc herniation with large annular defects had the most increased recurrence risk [8]. Other studies have shown that disc reherniation occurs more commonly in protrusion-type herniation [12] and subligamentous disc herniation [19]. In our study, extrusiontype disc herniation was more common than the protrusion type; however, this was not statistically significant. The degree of disc degeneration was related to the recovery rate of annulus fibrosus after discectomy [4]. Annular repair or leave may help reduce reherniation of disc, without increasing perioperative risk [7]; however, none of the patients in this study underwent annular repair. The results of a study revealed that disc reherniation is commonly noted at the L 4-5 level; however, it was not statistically significant [12]. Our study showed similar results.
Standard discectomy is more helpful in reducing reherniation of the disc compared to herniectomy, to a non-statistically significant degree [20]. Subtotal or aggressive discectomy (more resection of disc material after extruded or protruded disc removal) has a lower recurrent disc herniation rate than a limited discectomy. The overall outcome was still less satisfactory [3,21]. Persistent back or leg pain after discectomy is more common than limited discectomy [22]. However, the short-term follow-up results of less than two years did not differ between the two operative methods [21]. All patients in this study underwent subtotal discectomy.
Degenerative spine segments with preserved disc height are more prone to spinal instability than a collapsed disc [23]. A higher preoperative disc height is also a predisposing factor for recurrence [16]. After discectomy, the progression of disc degeneration may cause persistent back pain, especially in young patients, whereas maintaining disc height may increase the recurrence rate [24]. When the disc height decreases by more than 50%, the spine segment’s stability is improved [14]. In contrast, the progression of disc height decrease by more than 20% during follow-up was a statistically significant factor influencing recurrence of disc herniation in our study.
The occurrence of disc space narrowing after discectomy is common; however, the correlation with prognosis is not significant. Disc height index (DHI) and sagittal range of motion (sROM) are independent factors related to disc reherniation. More than 10° of sROM and high DHI induce reherniation [14]. Larger sROM and associated lumbosacral transitional vertebrae are independent risk factors for recurrent disc herniation [25].
Disc recurrence was more common on L 4-5 than on other levels [2,11]. Modic changes are strongly correlated with back pain, especially Modic I change [26], disc degeneration and severity of back pain [27]. Greater Modic endplate changes are risk factors for recurrence [16]. In our study, Modic change was not influenced by recurrence, while severe disc degeneration was influenced by recurrence; however, this was not statistically significant.
The relationship between facet joint degeneration and disc recurrence has yet to be discussed. Most facet joint degeneration appeared at the disc space level with advanced disc degenration [28]. Most cases of disc degeneration are preceded by facet joint degeneration. The appearance of facet joint degeneration induces increased disc loading, which may cause progression of disc degeneration [29]. Severe disc degeneration is also a predisposing factor for reherniation [2,4]. This mechanism of facet joint degeneration may influence disc recurrence.
Facet joint orientation and tropism may be important factors in inducing recurrent disc herniation. The incidence of recurrent lumbar disc herniation increases when facet orientation is decreased and facet tropism is decreased [30]. But, facet tropism did not correlate with facet joint degeneration [31]. Facet joint degeneration was a predisposing factor for recurrent disc herniation in our study.
Our study’s limitation is its retrospective design, variable follow-up periods, and that the volume of the removed disc was different in each case.
CONCLUSION
A disc space height decrease of more than 20% during the follow-up period, along with preoperative disc space height and facet joint degeneration grade 3 and 4 on Pathria’s classification were risk factors for disc reherniation. Patients who experienced preoperative facet joint degeneration at the operation site and progressive disc space height decrease during the follow-up period may require closer observation for disc reherniation.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.