INTRODUCTION
Lumbosacral extraforaminal stenosis (EFS) of the L5/S1, refers to narrowing of the L5 nerve root pathway. Nerve root pathway can be affected by various pathologic conditions, including extraforaminal herniated discs, osteophytes or fusion of the sacral ala and L5 transverse processes (TPs) [1]. This distinct pathologic phenomenon is also named as far-out syndrome, and sometime as a variant, it presents in the form of BertolottiŌĆÖs syndrome which indicates transitional vertebra of the lumbosacral junction [2]. While far-out syndrome indicates the degenerative change of the TP and sacral alar, the BertolottiŌĆÖs syndrome is rather a consequence following congenital anatomic variation of the L5/S1 segment [3,4]. Both occasionally result in back pain or radiculopathy of the L5 root. The incidence of extraforaminal stenosis has been reported to be 8% to 11% [5-7]. However, the diagnosis of this specific condition is sometimes challenging.
Imaging studies including X-ray, CT scans and MRI are the key diagnostic tool for L5/S1 EFS, of course accompanied with thorough physical examination [8]. As the compression of L5/S1 EFS occurs at the far lateral part of L5/S1 disc level, conventional MRI sagittal scans or axial scans can miss this region [9-13]. Coronal MRI is useful to check the degree of compression of the nerve root in EFS [14]. However, many patients with lumbar spondylosis undergo MRI scans that do not include a coronal view, and thus extraforaminal stenosis is sometimes overlooked.
In this report, we would like to introduce a case in which a patient who did not show improvement after several previous surgeries because of a misdiagnosed L5/S1 EFS and was eventually improved after a full endoscopic decompression surgery. Also, this case emphasizes the importance and significance of half coronal MRI scans in the diagnosis of this disease.
CASE REPORT
An 83-year-old male, visited our center complaining of back and left sided leg pain for the last 5 years. At the time of admission to our hospital, he had already undergone a total of 2 lumbar surgeries within the recent three years, all for the same symptom. He had two interbody fusion surgeries at the L3/4 and L4/5 levels, and also had several selective nerve root blocks and a percutaneous epidural neuroplasty (PEN) which only had transient pain relief effects. The left leg pain running down from the left buttock along the posterolateral thigh down to the lateral side of the ankle was noted, and due to this worsening pain, he was unable to ambulate. The initial physical examination revealed severe L5 dermatome radiating pain and paresthesia, accompanied ankle dorsiflexion weakness (Grade 3) which was clinically compatible with a left L5 radiculopathy.
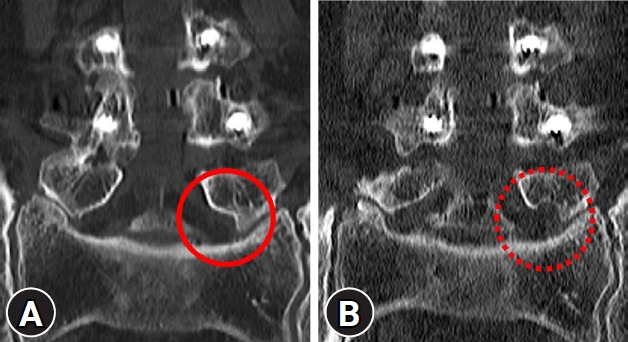
The patient reported that the current symptoms were present since the very beginning of the pain, and both of his prior surgeries (a L4/5 minimally invasive transforaminal lumbar interbody fusion; TLIF, and L3/4 oblique lumbar interbody fusion; OLIF) were done 3 years and 1 year before the visit, respectively. None of the fusion surgeries were helpful for his pain. On new the MRI scan, taken at our center, extraforaminal stenosis at the L5/S1 level was noted, with the L5 nerve root being significantly compromised between the caudal portion of the L5 transverse process (TP) and the sacral alar. The nerve root compression accompanied with consequent swelling was noted at the axial, sagittal and coronal images (Fig. 1).
Retrospectively reviewing the MRI scans from the previous surgeries, the L5/S1 extraforaminal stenosis might have been overlooked or neglected, probably because the axial and sagittal slices were not precisely taken at the right spot. Half coronal T1-weighted images which will be discussed in the later section are extremely helpful for the diagnosis of this specific pathology, however was not taken in the previous hospitals which could have led to the misdiagnosis of the stenosis.
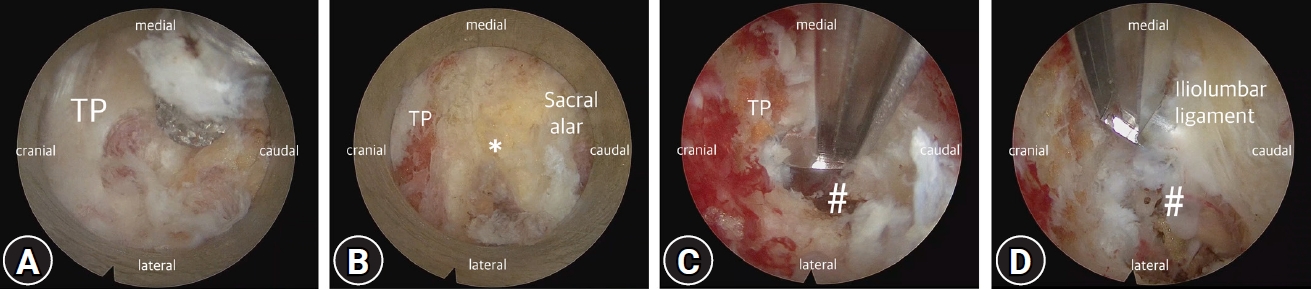
As the patient was suffering from intractable radicular pain not responding to further non-surgical procedures including selective L5 nerve root blocks or PEN, we consulted the patient and decided to perform a surgical decompression of the extraforaminal stenosis. As the patient was an old gentlemen with a history of angina and was under Edoxaban, we decided to perform a full-endoscopic decompression. With C-arm fluoroscopy assistance, one skin incision was made and serial dilators were inserted (Fig. 2). Uni-portal endoscopic spine surgery system (Joimax iLESSYS® Delta) was used for drilling out of the caudal one third of the TP and the rostral tip of the sacral alar. After adequate drilling of the TP-alar junction, the iliolumbar ligament was removed and the L5 nerve root was decompressed (Fig. 3). Postoperative CT scan presented successful resection of the TP, and the extraforaminal tract was widened indicating decompression of the L5 nerve root (Fig. 4). The patient reported immediate relief of leg pain, and was discharged 3 days after surgery. After 3 months, the patient reported 80% improvement of the radicular leg pain, 90% relief of back pain and is back to daily activities with improved ambulatory function.
DISCUSSION
Lumbosacral extraforaminal stenosis is caused by compression of the L5 root between the transverse process of the L5 lumbar spine and the ala of the sacrum. It was first reported in 1984 by Wiltse et al. [1], and named ŌĆśfar-out syndromeŌĆÖ because the nerve is compressed in the distal part outside the foramen. Since it is a narrowing of the space between the transverse process and the sacral ala, it is occasionally related to LSTV, which shows unspecified bone union at the lumbar sacral junction [2]. The far-out syndrome is different from LSTV or BertolottiŌĆÖs syndrome as they are consequences of degenerative changes rather than congenital characteristics [3,4]. Usually, disc levels under LSTV are known to be stable and less prone to degenerative changes, therefore the L5 radiculopathy related to this distinct anatomic location occurs more frequently in degenerative far-out syndromes [2,15].
Similar to most lumbosacral diseases that can cause radiculopathies, thorough physical examinations accompanied with adequate image studies are the standard diagnostic hallmarks [16]. Identifying symptomatic far-out syndrome occurring at the TP-alar junction starts from suspecting L5 radiculopathies by physical examinations. Afterwards structural and anatomic understanding based on the image studies are important. MRI is the diagnostic tool of choice since it can ideally identify disc space, spinal canal, paravertebral soft tissue, and CSF space [17,18]. Routine MRI exam shows sagittal and axial images with multiple image sequences and usually it is sufficient to make proper diagnosis. However, as the MRI image are slice images, MRI scans cannot fully cover the three-dimensional overall anatomic structures. Especially when only 2-dimensional axial, sagittal images are taken [10]. The use of half coronal MRI images in the diagnosis of extraforaminal stenosis was reported by Hashimoto et al. [14] and they reported that half coronal MR accurately visualize extraforaminal compression of nerve roots. Grenier et al. [12], reported that extraforaminal herniated discs not clearly identified on sagittal MR can be visualized on half coronal MR. In this case presentation, the initial L5 radiculopathy was neglected by previous surgeons and wrong level fusion surgeries were performed. In our institute, half coronal T1-weighted images are routinely performed in lumbar scans. Although well trained experienced physicians can still detect the far-out syndrome at the TP-alar junction with conventional axial/sagittal images, it can be missed or overlooked in MRI images with only sagittal and axial images [9-12]. In the early 1990s, many studies reported the high diagnostic value of half coronal plane in MRI in patients with lumbosacral extraforaminal stenosis [12,14]. MRI coronal views well present the pathway of nerve root narrowed due to the transverse process or osteophyte of the sacral ala or lumbosacral transitional vertebra, therefore are extremely valuable for the diagnosis of this distinct pathology [8,19]. Hashimoto, et al. [14], described nine patients with L5/S1 extraforaminal stenosis and highlighted the diagnostic value of MR imaging in the coronal plane. The use of half coronal image greatly benefits those with lesser experiences and the disease was well detected in this case presentation as we presented in the previous section.
Misdiagnosis of a L5/S1 extraforaminal far-out syndrome can lead to subsequent unnecessary surgeries which fail to alleviate the symptoms. The treatment of lumbosacral extraforaminal stenosis depend on severity of the symptoms [20]. The conservative treatment for extraforaminal stenosis is nerve block in addition to medication, and if conservative treatment is ineffective, surgery is considered. The key goal that must be achieved in the surgery for L5/S1 TP-alar far-out syndrome is the full removal of the structures causing impingement of the L5 nerve root [19]. Various surgical approaches or surgical techniques can be used according to the availability, or to the preference of surgeons. Many surgeons proposed various methods for surgery of extraforaminal stenosis or the L5/S1, including posterior midline approach, midline approach, anterior approach, and recently endoscopic approaches [1,3,5,13,19,21,22]. Recently, with the development of technology and endoscopic surgical instruments, a complete endoscopic approach, rather than microscopic surgery, has been attempted for decompression of the lumbar foramen and also the extraforaminal area of nerve roots [21]. Heo et al. [21] argues that bi-portal endoscopic surgery in far out syndrome has the advantages of minimally invasive surgery, such as minimizing trauma to the posterior muscle and ligament structures, reducing postoperative pain, and promoting recovery after surgery, while the results are not significantly different from those of open surgery. Although we took a uni-portal endoscopic approach, it is considered that the results are not significantly different from their results in terms of full endoscopic decompression. Also, Khoo and Fessler [22] reported that blood loss for endoscopic approach group was less than 30% of that of the open surgery group. In this case report, we successfully decompressed the L5 root by fully removing the caudal half of the TP and also the cranial part of the sacral alar by full-endoscopic technique. This minimally invasive technique can be especially feasible for patients whom have high peri-operative risks, or for those under anticoagulants or antiplatelets due to medical conditions, over the open surgery [22].
Extraforaminal stenosis at the TP-alar junction of L5/S1 is a distinct pathology which occasionally leads to significant L5 radiculopathy. Due to the anatomic nature of the disease, it can be easily missed on routine axial and sagittal MRI scans without the half coronal view. Therefore, it is necessary to include the coronal view in MRI to avoid possible misdiagnosis of the disease. We have shown that full endoscopic uni-portal approach is a useful surgical method for these lesions.