Clinical Importance of Hounsfield Unit in Computed Tomography of Sub-Axial Cervical Vertebral Body.
Article information
Abstract
Objective
Computed tomography (CT) is an often-used diagnostic imaging tool during the evaluation of the cervical spine pathology. CT scan can provide one’s bone density by measuring Hounsfield’s unit. In anterior cervical discectomy and fusion (ACDF) surgeries, bone density may play an important role as it may relate to non-union. Therefore, the evaluation and consideration of the Hounsfield’s unit of sub-axial cervical vertebral body is important, especially during multi-level ACDF.
Methods
Patients who have taken cervical CT scan pre-operatively to multi-level (3 or 4 levels) anterior cervical discectomy and fusion with anterior plating between June 2010 and August 2018, at our department were retrospectively reviewed. The bone density was estimated by measuring Hounsfield Unit (HU) of sub-axial vertebrae - C3 to T1 - by using PiViewStar imaging software program. Radiological evaluation of fusion was done by assessing postoperative plain X-rays and CT scans of 4 months and 1-year follow-up. The difference in HU were evaluated between different segments of sub-axial vertebrae. Then the fusion rate of the ACDF ending at C6 were compared to C7. All grouped values were tested for normality using the Shapiro-Wilk test. Matched-ANOVA and Fisher’s exact test was used.
Results
A total of eighty patients were who underwent 3 or 4 level ACDF with anterior plate fixation were retrospectively reviewed. Bone density estimated from Hounsfield unit (HU) measurement of the sub-axial vertebral bodies ranges from 112.2 to 594.9 with the mean of 280.91. When comparing C5 with 6, 6 with 7, and 7 with T1 they showed significantly decreasing HU value with p-value<0.01 with mean difference of 49.10, 30.98, and 31.25, respectively. ACDF ending at C7 showed significantly lower fusion rate than C6 at 4 months and 1-year follow-up, respectively.
Conclusion
The HU show a decreasing trend towards lower sub-axial cervical vertebral body. Furthermore, multi-level ACDF ending at C7 showed higher non-union rate than ending at C6. Although, there is no direct evidence that lower bone density at lower sub-axial cervical vertebrae is causative for non-union, it should be considered for pre-operative planning.
INTRODUCTION
Computed tomography (CT) is an often-used diagnostic imaging tool during the evaluation of the cervical spine pathology [1]. While magnetic resonance imaging has its advantage on soft-tissue contrast, CT scan better depicts bony parts. In CT scan, the attenuation of x-ray beam is calculated for each voxel in Hounsfield unit (HU) to represent the radiodensity quantitively [2]. The value of HU varies in different tissues as well as within bony parts, which usually ranges from 300 to 3,000 [3].
Bone density is an important aspect of pre-operative surgical planning. DEXA and QCT is frequently used tool to estimate the bone density of the spine, however, limited evidences are provided for the cervical spine [4]. The use of the HU value of the CT scan to estimate the bone density is gaining more acceptance in recent times among spine surgeons, as CT scan is often available pre-operatively and most commercially available image viewers can calculate the mean HU value at the region of interest (ROI) [5,6].
Anterior cervical discectomy and fusion (ACDF) with plating is a widely performed procedure for cervical disc diseases [7,8]. Although promising clinical results are widely reported, non-union related complications such as instrument failure and associated neurologic deficit or pain. In patients with osteoporosis, non-union is more likely to occur as fixated implants are more easily loosened [9]. Single or two level ACDFs infrequently result in non-union and numerous studies have reported fusion rate up to 100% [10,11]. However, multi-level ACDFs have higher complication rate [12,13]. Therefore, a careful preoperative evaluation is needed regarding the bone density, and accordingly cautious surgical strategies may be necessary to reduce the non-union rate.
In this study, the authors aimed to evaluate the HU values in different level of sub-axial cervical vertebral bodies. Subsequently, non-union rate and affected segment level will be evaluated. The ultimate goal of this study is to reinforce the surgical strategies and reduce complications caused by non-union based on the characteristics of HU values in different levels of sub-axial vertebral bodies.
MATERIALS AND METHODS
1. Patient Population
This study was approved by the Institutional Review Board of Korea University Medicine (No. 2021GR1336). Patients who have taken cervical CT scan pre-operatively to multi-level (3 or 4 levels) anterior cervical discectomy and fusion with anterior plating between June 2010 and August 2018, at our department were retrospectively reviewed. Electronic medical records (EMR) and Picture Archiving and Communication System (PACS) used at the hospital were reviewed to collect clinical and radiologic data, respectively. Patients who underwent other surgical procedures besides ACDF, such as corpectomy or additional posterior fixations, were excluded from the study. Patients who could not be followed or who received early revision surgery were also excluded from the study.
2. Radiological Evaluations
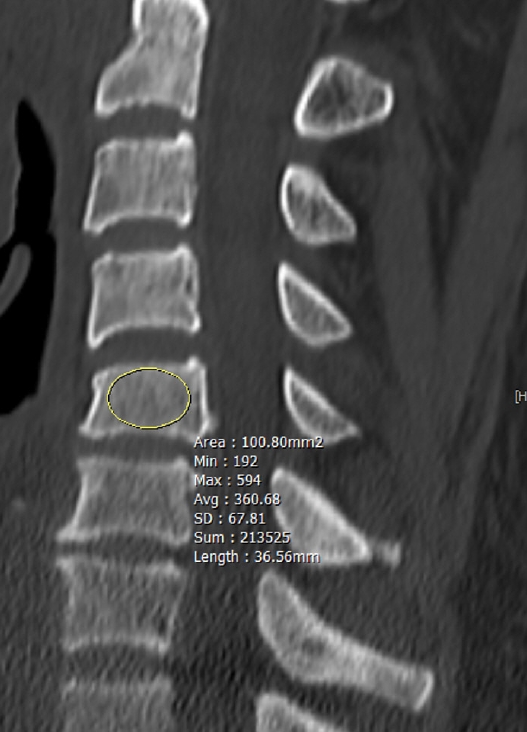
The bone density was estimated by measuring Hounsfield Unit (HU) of sub-axial vertebrae - C3 to T1 - by using PiViewStar imaging software program. Region of interest (ROI) was drawn at cancellous bone of the body on a mid-sagittal view (Fig. 1). ROI was devoid of cortical bone, any osseous abnormalities, and density void caused by basivertebral foramen.
Radiological evaluation of fusion was done by assessing postoperative plain X-rays, and when the plain X-rays was ambiguous to judge, cervical CT scan was used to confirm. Anteroposterior (AP), lateral and flexion/extension lateral plain radiographs were taken prior to the surgery, and then followed at 4, 12, and 24 months after the operation. All X-rays and CT scans were evaluated by 2 neurosurgeons. Fusion was confirmed by: (i) the absence of motion >2 mm between the tips of spinous processes on flexion/extension lateral radiographs; (ii) the absence of a radiolucent gap between the graft and the endplate; and (iii) the presence of continuous bridging trabeculae at the graft and endplate junction. Assessment for fusion were done at each operated interbody (Fig. 2).

Post-op 1 yr f/u X-ray image. (A) Flexion image and (B) extension image of non-union case. It is cervical X-ray image of C4 to 7 ACDF. At proximal portion, radiolucent gap was suspected between the graft and the endplate (circles). In the flexion-extension comparison, the spinous tip is accompanied by a motion of more than 2 mm. In this case, the mean value of hounsfield units measured by pre-op CT was 293.71. (C) Flexion image and (D) extension image of union case. There is no motion between the tips of spinous process, there are no radiolucent fissures, and the continuity of the bones is well identified. In this case, the mean value of hounsfield units measured by pre-op CT was 176.53.
3. Statistical Analysis
All statistical analyses were performed using SPSS (version 20; SPSS, Chicago, IL, USA), and statistical significance was defined as p<0.05. All grouped values were tested for normality using the Shapiro-Wilk test. Matched-ANOVA was used to test the differences in HU value in different level of sub-axial cervical spine. Post-hoc test was done using student’s t-test or Mann-Whitney test depending on the normality of the data.
RESULTS
1. Demographics
A total of eighty patients were who underwent 3 or 4 level ACDF with anterior plate fixation were retrospectively reviewed. Of those, 67 patients underwent 3 level ACDF (16 females, 51 males; mean age, 54.1±9.85 years; age range, 32–72 years) and 13 patients underwent 4 levels (4 females, 9 males; mean age, 55.50±9.12 years; age range, 41–70 years) with a total operated segment of 253 (Table 1). The mean post-operative follow-up period was 1.8 years. 9 patients were missed at 1-year follow-up - 8 patients did not present and one patient underwent revisional operation - and 19 patients were cumulatively missed at 2-year follow-up (Fig. 3).
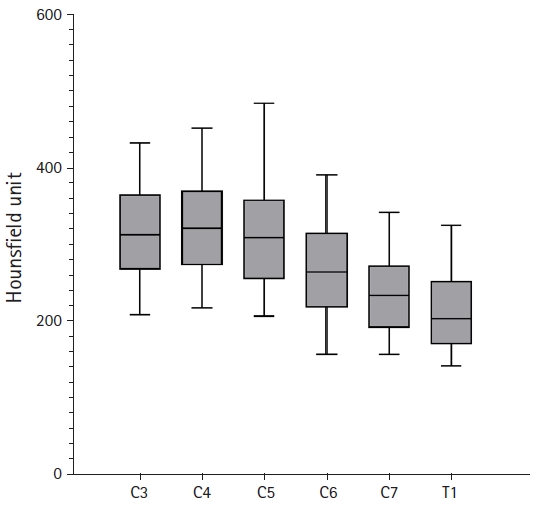
2. Hounsfield Unit of Sub-Axial Vertebral Bodies
Six of eighty patients were excluded in Hounsfield unit (HU) measurement due to no CT evaluation at pre-operation. Bone density estimated from HU measurement of the sub-axial vertebral bodies ranges from 112.2 to 594.9 with the mean of 280.91. HU values are largely variable within each vertebral level with standard deviation ranging between 58.03 and 78.16 (Table 2). However, an obvious trend in HU values can be observed in sub-axial vertebrae. The trend analysis of the HU along decreasing order of vertebral level is significant for both linear, quadratic and cubic trend with p-value of <0.01. Pairwise comparisons of HU in sub-axial vertebrae show a similarity in HU value at C5 with C3 and C4 with p-value of 0.305 and 0.356, respectively. However, when comparing C5 with 6, 6 with 7, and 7 with T1 they showed significantly decreasing HU value with p-value<0.01 with mean difference of 49.10, 30.98, and 31.25, respectively (Table 3, Fig. 4).
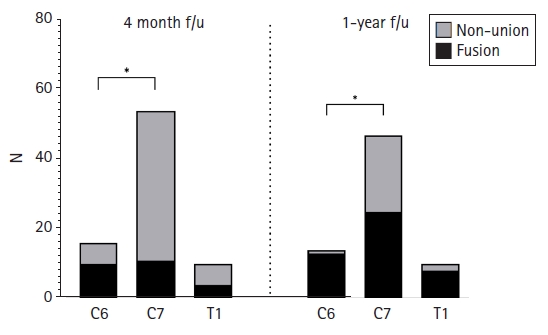
3. Fusion Rate
Overall fusion rate of the 80 patients in this study were 31.3% at 4 months, 54.9% at 1 year, and 75.4% by 2-year follow-up. All of non-union occurred at the most caudal segments of the construct (Table 4). At 4 months follow-up, 10 out of 16 patients (62.5%) with ACDF at C3-6, 11 out of 54 patients (20.4%) with ACDF caudally ending at C7 (mean of 3.2 operated segments) and 4 out of 10 patients with ACDF caudally ending at T1 (mean of 3.2 operated segments). During the follow-up, the fusion rate of ACDF caudally ending at C6, C7, and T1 gradually increased to 85.7, 46.8 and 50.0% by 1 year and 100, 64.1 and 88.9% by 2 years, respectively (Table 5, Fig. 5). Notably, fusion rate of ACDF caudally ending at C7 were poor compared to C6.
DISCUSSION
Hounsfield unit is frequently used to estimate bone density in the cervical vertebrae, which may give important information for surgical planning. The correlation between the value of HU values and the bone mineral density (BMD) of the spine were reported in the several previous papers [5,14]. A study regarding volumetric BMD (vBMD) on the cervical spine reported the gradually decreasing bone density below C4 [4,15]. In accordance to their study, we have measured the HU of C3 to T1 vertebral bodies from the cervical CT scans. The results are similar to their study as shown in the Table 2. Therefore, bone density estimation can be compatible with the measurement of HU value from the CT scan. Furthermore, assumption can be made regarding gradually decreasing BMD at the lower cervical vertebral bodies that it may relate to an increased rate of postoperative non-union. Conversely, the high fusion rate in the upper cervical vertebrae of C6 or upper may be explained.
Multi-level ACDF involving 3 or more levels, have been performed since late 90’s and fusion rate reported in literatures are 47% to 100% [8,16-19]. However, the criteria for fusion are arbitrary in current studies and poorer fusion rates had been reported in recent years [20]. Subsequently, a high clinic-economical burden of non-union in ACDF was also reported [21]. Although non-union does not necessarily correlate with poor clinical outcome, the long-term consequence of non-union is uncertain and consideration for a revision operation is often an issue [22]. The occurrence of non-union was rarely seen in the middle segment, and most occurred in the proximal most and the distal most end segments, especially in the most distal segment [7,23]. Papadopoulos et al. have reported that their the non-union cases (2 out of 46 cases) were all non-union of caudal most levels and this study also confirmed the same results [24]. The occurrence of the non-union only at both ends could be induced by the motion generated in the upper and lower parts of the surgically fixed segment, but the cause of the non-union especially in the most distal segment was unknown. Despite of the non-union, there was a high structural stability due to the internal fixation through the anterior plate system using screw, and the clinical outcomes improved [25]. Therefore, if there were no definite symptoms that the patient needed to re-visit in the hospital, the loss in the long-term follow-up was increased despite the non-union [26]. However, in the state of absence of bony fusion, bone remodeling and absorption occur between the inserted bone grafts and the surrounding vertebrae in the operated segment. In addition, repetitive motion at the non-union site causes a degenerative change of the vertebra around the instruments. Structurally, the instability gradually increase as the inserted bone grafts collapses or the graft progresses subsidence into the end plate [10]. This instability caused by the non-union of the operative segments can sometimes lead to damage to the plate system, which in turn weakens the fixative force produced by the plate using screw [27]. As a result, screw pull-out or breakage may occur due to the change of the force applied to the screw, which accelerates the deterioration of the plate system instability and causes an instrument failure or telescoping in which the entire surgical segment is collapsed [10,28]. In rare cases of catastrophic instrument failure may require reoperation in long-term non-union [29,30].
In this study, we found that the fusion rate was significantly lowered when the multi-level ACDFs contained C7 or below segments and there were two cases that needed revision operation due to instrument failure. The first case was minimal extrusion of distal screws in the plating system. The patient complained of axial pain in the neck. We decided a re-operation and performed posterior interspinous screw fixation at most distal segment, at C6/7, and the patient’s symptoms improved. In another case, revision was done at 6 post-operative months because the proximal screw at C3 was broken and movement occurred at the upper segments. Posterior screw augmentation resulted in a solid fusion in the segment. All of the two reoperation cases were performed in the early stages of the study; therefore, the authors were uncertain of the consequences that may resulted from instrument failure. However, since the upper cervical segments has a relatively high bone density, fusion is likely to occur. Therefore, the revision operation might have been unnecessary. On the other hand, non-unions in the distal segments may need more careful manipulations as it may cause persisting clinical symptoms. The distal non-unions may be prevented by using thicker screws at the distal end of the construct bi-cortically. Moreover, leaving space below the anterior plate with appropriate cortical bone preparation may induce bone growth around the plate, providing extra stability to the construct.
This study has some limitations. Because of the relatively rare cases of multi-level ACDFs, data from a single center were collected for 8 years, but relatively few cases were available to prove accurate statistical results. Furthermore, cases often lost during follow-up and there was additional loss of data compared to the total number of surgical cases performed at the final follow-up. An additional multicenter study including larger number of patients might be a solution to overcome this problem. Another issue is the determination of successful fusion. In spite of the criteria for fusion that is similar to the previously published paper, the difference in the final fusion rate compared to other previously published papers was significant. The difference in these results suggests that our study may have applied more strict judgment on successful fusion. Further discussion of the criteria for clear and more accurate bony fusion may be needed. Moreover, this study cannot give a direct correlation between the HU value and the fusion rate. Therefore, further studies are needed to conclude that there is a causal relationship.
CONCLUSION
The HU measurement in sub-axial vertebral bodies show a decreasing trend towards lower segments. Most non-union occur at caudal most segments of multi-level ACDF and constructs ending at C7 showed higher non-union rate than ending at C6. Although, direct relationship between HU and non-union rate cannot be determined from this study, given the information, constructs ending below C6 need more careful surgical strategies to prevent from non-union. Conversely, early interventions in asymptomatic non-unions in the middle or upper segments of the multi-level ACDF constructs can be delayed, as eventual fusion can be anticipated.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.